Restrictive Practices
A printable version of this article is available for download at the bottom of this page.
What are Restrictive Practices?
A restrictive practice occurs when a child is denied or has restricted access to an item, activity or experience as a means of limiting a behaviour. Under the UN Convention on the Rights of the Child a child holds the right to live free from abuse and harm and, to feel safe and supported within their environment. In response to the Rights of the Child, the NSW Care and Protection Act requires that carers manage children’s behaviours subject to regulations, and implement therapeutic parenting. For example, confiscating a child's iPad [that is their own possession] is a restrictive practice and would require a modified response by the caregiver.
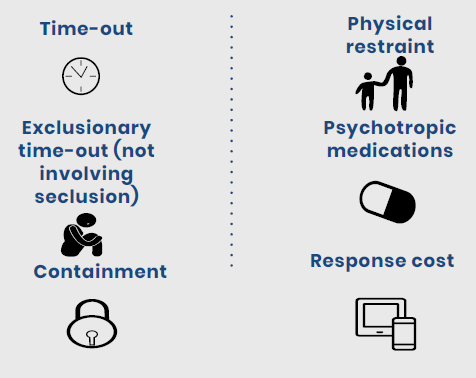
What counts as a restrictive practice?
The following point are all counted as restrictive practices.
Psychotropic Medications
A psychotropic medication is any drug which affects behaviour, mood, thoughts, or perception (Ghoshal, 2019). This class of medications can be used to treat conditions such as anxiety, ADHD or sleep disorders. Psychotropic medications are considered chemical restraint; therefore, in cooperation with the child’s agency, a treatment plan must be devised. A treatment plan should outline the type of drug, how frequent and the dosage at which it is taken, and a review date by a health professional. In conjunction with medication, a treatment plan should include holistic strategies to support the child’s health and wellbeing.
Restricted Practices as a Crisis Response
A crisis response occurs when a restricted practice is used and is not informed by a positive behaviour support plan. Restricted practices without a plan are considered reportable conduct and should be followed up by:
Speaking to a caseworker – providing information about what happened.
Involving the child in therapeutic interventions.
Engaging in carer support.
Positive Behaviour Support Plans
A positive behaviour support plan is a person-centred document which outlines how to support behaviour change in children requiring a restrictive practice. Like a treatment plan, PBSP's are collaboratively developed by the agency, carer, and most importantly the child. A PBSP is based around goal setting and consideration of the likes/dislikes of the child. The function of a PBSP is to identify:
What are the behaviours a function of?
What do we need to work on?
Where did it originate? i.e. trauma? executive functioning?
After its implementation a PBSP should be monitored by the carer of the child and reviewed every 3 months. It is anticipated that as children heal from trauma or settle into a placement, the severity of behaviours should reduce over time.
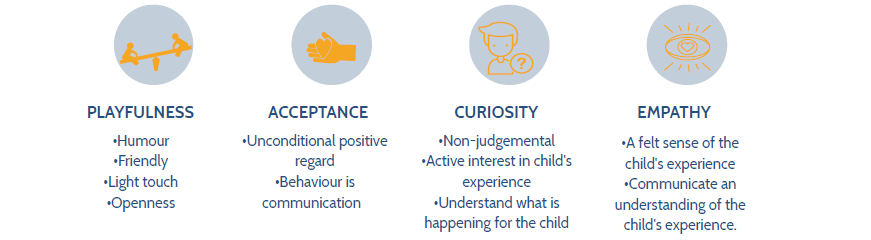
Using the P.A.C.E Model
Dan Hughes’ P.A.C.E model is a therapeutic parenting approach in which carers can support children in developing self-awareness and regulating emotions. While we cannot undo a child’s experience of trauma, promoting a PACE model can alter the way children respond to the impacts of their trauma.
Identifying Triggers
Changes to routine
Perception of fairness
Doing things they do not want to do
Unplanned surprises
Distraction by others
Not feeling heard
Preventing Dysregulation
Prompt the child before an activity change
Maintain routine
Listen
Maintain attunement and focus on the child - focus on other tasks/people can be perceived as rejection
Reactive Vs. Responding
Reacting: Meeting the child’s emotionally-charged behaviour with an emotionally-charged reply
Responding: Allowing the child to express big emotions, ideas and, feelings without criticism, shame or, guilt
Caring for Indigenous Children
Physical punishment is not acceptable or effective
Understand the historical context around humiliation, restraint and, intimidation
Reciprocal respect
Download the free printable of this article here.